Trauma Induced Schizophrenia Links Explored

- 1.
Understanding the Complex Relationship Between Trauma and Schizophrenia
- 2.
What Does the Research Actually Say About Trauma Induced Schizophrenia?
- 3.
Common Types of Trauma Associated with Schizophrenia Development
- 4.
Distinguishing Between Trauma-Induced Psychosis and Primary Schizophrenia
- 5.
How Long Does Trauma-Induced Psychosis Typically Last?
- 6.
Can Extreme Stress Actually Cause Schizophrenia?
- 7.
Best Lifestyle Approaches for Managing Schizophrenia Symptoms
- 8.
What Is the 25 Rule for Schizophrenia?
- 9.
Treatment Options for Trauma Induced Schizophrenia
- 10.
Additional Resources and Support for Understanding Trauma Induced Schizophrenia
Table of Contents
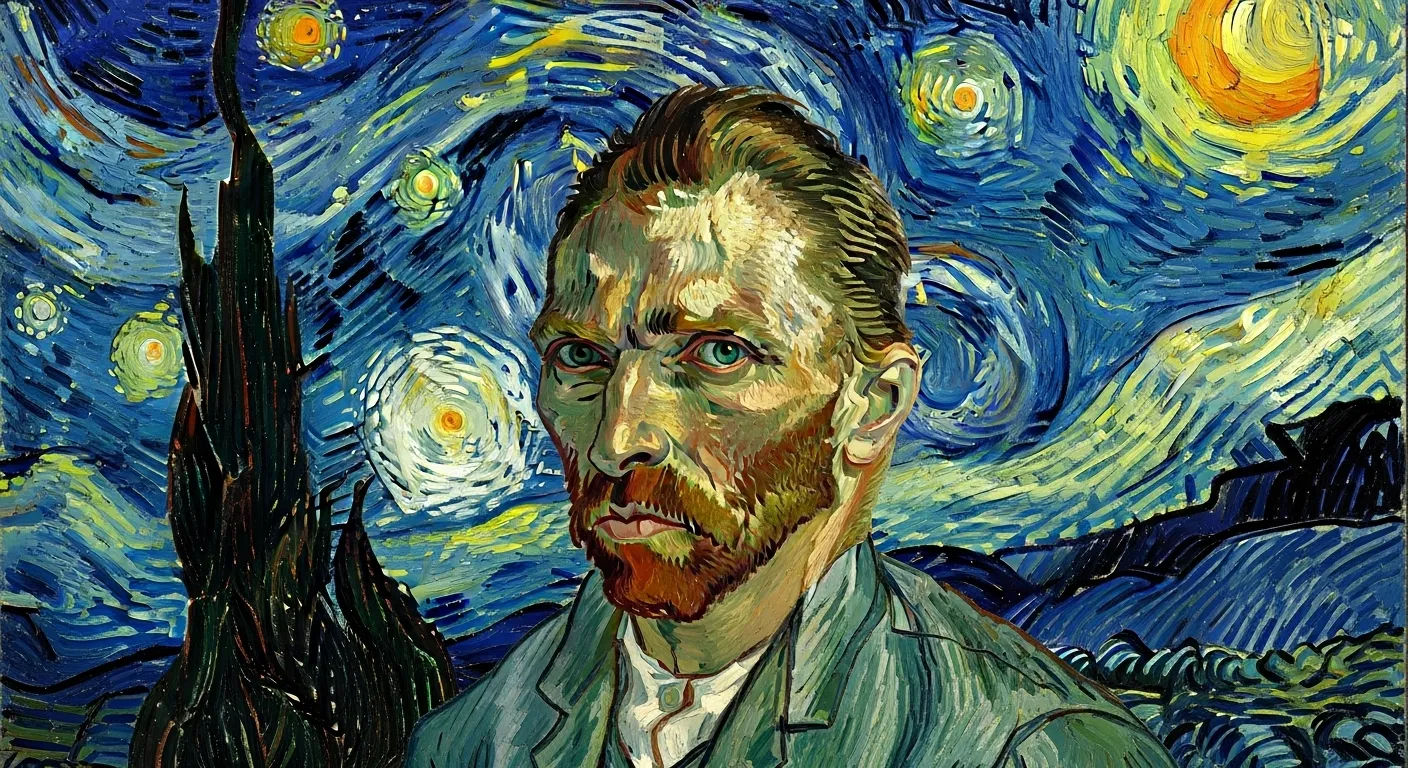
trauma induced schizophrenia
Understanding the Complex Relationship Between Trauma and Schizophrenia
Alright, let's get real about this whole trauma induced schizophrenia situation. First things first—schizophrenia ain't just some made-up Hollywood drama where people see things that ain't there (though that can be part of it). It's a legit brain disorder that affects how folks think, feel, and perceive reality. Now, when we talk about trauma induced schizophrenia, we're lookin' at cases where severe psychological trauma might've triggered or worsened the condition in folks who were already genetically predisposed. Think of it like this: genetics loads the gun, but environment pulls the trigger. Trauma—whether it's childhood abuse, combat exposure, or witnessing something horrific—can be that trigger for some people. But here's the kicker: not everyone who experiences trauma develops schizophrenia, and not everyone with schizophrenia has a trauma history. It's complicated, messy, and deeply personal for each individual walkin' this path.
What Does the Research Actually Say About Trauma Induced Schizophrenia?
So what's the science got to say about trauma induced schizophrenia? Well, buckle up, 'cause the research is pretty eye-openin'. Studies show that folks who've experienced severe childhood trauma are about 2-3 times more likely to develop schizophrenia later in life compared to those who haven't. That's not small potatoes! A massive meta-analysis published in the Schizophrenia Bulletin found that nearly 70% of people diagnosed with schizophrenia reported at least one traumatic event in their lifetime—way higher than the general population. But correlation ain't causation, right? The brain science gets even more interestin': trauma can actually change how your brain develops, particularly in areas responsible for stress regulation and emotional processing. This might explain why some folks with trauma histories are more vulnerable to psychotic episodes when life throws 'em a curveball. The research on trauma induced schizophrenia is still evolvin', but one thing's clear—trauma matters, and it deserves way more attention in how we understand and treat this condition.
Common Types of Trauma Associated with Schizophrenia Development
When we're talkin' about trauma induced schizophrenia, we ain't just talkin' about one specific type of trauma—there's a whole spectrum of experiences that can potentially play a role. Childhood abuse (physical, sexual, or emotional) tops the list, with studies showin' it's particularly impactful during those critical developmental years. But it ain't just about what happens when you're a kid—adult trauma like combat exposure, serious accidents, natural disasters, or witnessing violence can also be factors. Even chronic stress and discrimination over time can wear down your brain's resilience in ways that might contribute to trauma induced schizophrenia. The key thing to remember is that trauma is subjective—what's traumatic for one person might not be for another, and that's totally valid. Your brain's response to trauma is as unique as your fingerprint, and understanding that individuality is crucial when we're talkin' about mental health.
Distinguishing Between Trauma-Induced Psychosis and Primary Schizophrenia
Here's where things get tricky—how do you tell the difference between trauma induced schizophrenia and schizophrenia that develops without obvious trauma? Honestly, even the experts sometimes scratch their heads over this one. Trauma-induced psychosis often has a clearer timeline—you can usually pinpoint when the traumatic event happened and when symptoms started showin' up. It might also include more flashbacks or trauma-related content in the hallucinations or delusions. Primary schizophrenia, on the other hand, tends to have a more gradual onset and might include symptoms that don't seem directly connected to any specific trauma. But here's the real talk: these categories ain't always neat and tidy. Many folks have both genetic vulnerability AND trauma history, making it a real mixed bag. The good news? Treatment approaches are often similar regardless of the exact cause, focusing on managing symptoms and improving quality of life for folks livin' with trauma induced schizophrenia.
How Long Does Trauma-Induced Psychosis Typically Last?
This is one of those million-dollar questions, ain't it? How long does trauma induced schizophrenia or trauma-induced psychosis actually stick around? Well, the honest answer is: it depends. For some folks, trauma-induced psychotic episodes might be relatively short-lived—maybe lasting weeks or months with proper treatment. For others, particularly those with underlying genetic vulnerability, symptoms might persist longer or even become chronic. Research suggests that trauma-induced psychosis often has a better prognosis than primary schizophrenia, especially when the trauma is addressed directly in treatment. But recovery ain't linear—there might be ups and downs, good days and not-so-good days. The important thing is that with the right support and treatment, many folks experiencing trauma induced schizophrenia can learn to manage their symptoms and live fulfilling lives. It's not about "getting over it" overnight; it's about building resilience and finding what works for you.

Can Extreme Stress Actually Cause Schizophrenia?
Let's tackle this head-on: can extreme stress alone cause trauma induced schizophrenia? The short answer is probably not in most cases—but it's complicated. Think of schizophrenia like a three-legged stool: you've got genetics, brain chemistry, and environmental factors (including trauma and stress). If you're missing one leg, the stool might wobble but it probably won't collapse. Extreme stress alone is unlikely to cause full-blown schizophrenia in someone with no genetic predisposition. However, for folks who are already vulnerable, extreme stress can definitely be the straw that breaks the camel's back. It's like having a genetic time bomb that needs a trigger—and extreme stress or trauma can be that trigger. The research shows that chronic stress can actually change your brain chemistry in ways that might increase vulnerability to psychotic disorders. So while stress alone might not cause trauma induced schizophrenia, it's definitely a piece of the puzzle that deserves serious attention.
Best Lifestyle Approaches for Managing Schizophrenia Symptoms
Alright, let's get practical—what's the best lifestyle for someone dealin' with trauma induced schizophrenia or any form of schizophrenia? First and foremost: consistency is your best friend. Regular sleep patterns, balanced meals, and daily routines can work wonders for stabilizing mood and reducing symptom severity. Exercise ain't just good for your body—it's legit medicine for your brain, releasing those feel-good chemicals that can help counteract some of the negative symptoms of schizophrenia. Social connection matters too, even when it feels like the last thing you wanna do. Isolation can make symptoms worse, so finding your people—whether that's family, friends, or support groups—is crucial. Oh, and let's talk about substances: alcohol and drugs might seem like a temporary escape, but they'll almost always make things worse in the long run. The best lifestyle for trauma induced schizophrenia is one that prioritizes stability, self-care, and connection while avoiding things that can trigger or worsen symptoms.
What Is the 25 Rule for Schizophrenia?
You might've heard folks talkin' about the "25 rule" for schizophrenia, and honestly, it's one of those things that gets thrown around a lot but ain't always explained clearly. The basic idea is that about 25% of people diagnosed with schizophrenia will have a single episode and never experience symptoms again, another 25% will have recurring episodes but can maintain relatively normal functioning between them, and the remaining 50% will have more chronic, persistent symptoms. But here's the thing about trauma induced schizophrenia—this rule might not apply as neatly. Trauma-induced cases often have different trajectories, sometimes with better outcomes when the underlying trauma is properly addressed. The "25 rule" is more of a rough guideline than a hard-and-fast prediction, and individual outcomes can vary widely based on factors like access to treatment, social support, and how well trauma is integrated into the recovery process. Don't let statistics define your journey with trauma induced schizophrenia—every person's path to wellness is unique.
Treatment Options for Trauma Induced Schizophrenia
When it comes to treatin' trauma induced schizophrenia, it ain't a one-size-fits-all situation. Medication is often part of the equation—antipsychotics can help manage symptoms like hallucinations and delusions, while antidepressants or anti-anxiety meds might help with trauma-related symptoms. But meds alone ain't enough, especially when trauma's in the picture. Therapy is where the real magic happens: approaches like trauma-focused cognitive behavioral therapy (TF-CBT) or eye movement desensitization and reprocessing (EMDR) can help folks process traumatic memories in a safe, controlled way. Family therapy can be crucial too, helping loved ones understand what's goin' on and how to provide support without enabling unhealthy patterns. For trauma induced schizophrenia, the most effective treatment plans usually combine medication, trauma-specific therapy, and strong social support. It's about treating the whole person, not just the symptoms.
Additional Resources and Support for Understanding Trauma Induced Schizophrenia
Navigating the world of trauma induced schizophrenia can feel overwhelming, but you don't have to do it alone. Knowledge is power, and there are tons of resources out there to help you understand what you or your loved one might be experiencing. For comprehensive information about mental health conditions and their connections, visit the Twitch Documentary homepage, explore our Mental category for related topics, or dive deeper into biological factors with our article on Toxoplasmosis Schizophrenia Connection. Support groups, both online and in-person, can provide connection with others who get what you're going through. And remember—recovery is possible. With the right treatment, support, and self-care, many folks living with trauma induced schizophrenia lead meaningful, fulfilling lives. Your story ain't over—it's just entering a new chapter.
Frequently Asked Questions
What is the best lifestyle for schizophrenia?
The best lifestyle for schizophrenia includes maintaining consistent daily routines, getting regular sleep (7-9 hours per night), eating balanced meals with limited processed foods, and engaging in regular physical activity. Social connection is crucial—maintaining relationships with supportive family and friends can significantly improve outcomes. Avoiding alcohol and recreational drugs is essential, as these can worsen symptoms and interfere with medication effectiveness. For those with trauma induced schizophrenia, incorporating trauma-informed self-care practices like mindfulness, journaling, and creative expression can be particularly beneficial. Working closely with healthcare providers to develop a personalized wellness plan is key to managing schizophrenia effectively.
What is the 25 rule for schizophrenia?
The "25 rule" for schizophrenia refers to a general prognosis guideline suggesting that approximately 25% of people diagnosed with schizophrenia will experience only one psychotic episode and recover fully, another 25% will have recurring episodes but maintain good functioning between episodes, and the remaining 50% will have more chronic, persistent symptoms requiring ongoing management. However, this rule is a rough estimate and individual outcomes vary widely based on factors like access to treatment, social support, and whether trauma is involved. For trauma induced schizophrenia, outcomes may differ, particularly when trauma is addressed directly in treatment, potentially leading to better recovery rates than the general schizophrenia population.
How long does trauma-induced psychosis last?
The duration of trauma-induced psychosis varies significantly depending on individual factors. For some people, symptoms may resolve within weeks to months with appropriate treatment, particularly when the underlying trauma is addressed. Others may experience longer-lasting symptoms, especially if there's an underlying genetic vulnerability to psychotic disorders. Research suggests that trauma-induced psychosis often has a better prognosis than primary schizophrenia when trauma-focused treatment is provided. Early intervention is crucial—seeking help as soon as symptoms appear can significantly improve outcomes. With proper treatment including medication, trauma therapy, and social support, many people experiencing trauma induced schizophrenia can achieve significant symptom reduction and improved functioning over time.
Can extreme stress cause schizophrenia?
Extreme stress alone is unlikely to cause schizophrenia in someone without genetic predisposition, but it can definitely trigger the onset of symptoms in vulnerable individuals. Schizophrenia typically results from a combination of genetic factors, brain chemistry abnormalities, and environmental triggers—including severe stress or trauma. Chronic extreme stress can alter brain chemistry and structure in ways that may increase vulnerability to psychotic disorders. For people with trauma induced schizophrenia, extreme stress often serves as the environmental trigger that activates underlying genetic vulnerability. While stress management alone won't prevent schizophrenia in high-risk individuals, reducing chronic stress and addressing trauma can be important components of both prevention and treatment strategies.
References
- https://www.nimh.nih.gov/health/statistics/schizophrenia
- https://www.psychiatry.org/patients-families/schizophrenia
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5478535/
- https://www.who.int/news-room/fact-sheets/detail/schizophrenia