Paranoid Schizophrenia Dsm 5 Criteria

- 1.
Understanding the Evolution of Paranoid Schizophrenia in DSM-5
- 2.
What Paranoid Schizophrenia Looked Like Before DSM-5 Changes
- 3.
Why the DSM-5 Eliminated Paranoid Schizophrenia as a Separate Diagnosis
- 4.
Current DSM-5 Criteria for Schizophrenia Diagnosis
- 5.
Recognizing Paranoid Features in Current Schizophrenia Diagnoses
- 6.
Common Signs and Symptoms of Paranoid Schizophrenia Presentation
- 7.
The Diagnostic Process: How Clinicians Assess Schizophrenia
- 8.
Differential Diagnosis: Conditions That Mimic Paranoid Schizophrenia
- 9.
Treatment Approaches for Schizophrenia with Paranoid Features
- 10.
Living with Schizophrenia: Support Systems and Recovery
Table of Contents
paranoid schizophrenia dsm 5
Understanding the Evolution of Paranoid Schizophrenia in DSM-5
Here's the thing about paranoid schizophrenia dsm 5—it doesn't actually exist as a separate diagnosis anymore, and that's probably got you scratchin' your head like a confused puppy. Back in the day (we're talkin' DSM-IV era), paranoid schizophrenia was its own special category, like the VIP section of schizophrenia diagnoses. But when the American Psychiatric Association rolled out DSM-5 in 2013, they decided to shake things up and consolidate all those subtypes—paranoid, disorganized, catatonic, residual, and undifferentiated—into one unified diagnosis: schizophrenia. The reasoning? Those subtypes weren't really holdin' up in the real world; patients kept bouncin' between categories like ping-pong balls, and treatment approaches didn't really change based on the subtype anyway. So now when we talk about paranoid schizophrenia dsm 5, we're really talkin' about schizophrenia with prominent paranoid features, not a separate diagnosis altogether.
What Paranoid Schizophrenia Looked Like Before DSM-5 Changes
Before we dive into the current paranoid schizophrenia dsm 5 landscape, let's take a quick trip down memory lane to understand what paranoid schizophrenia used to mean. Under the old system, paranoid schizophrenia was characterized by prominent delusions (usually persecutory or grandiose) and frequent auditory hallucinations, but with relatively preserved cognitive functioning and affect. Unlike other subtypes, folks with paranoid schizophrenia typically maintained better organization in their thoughts and behaviors—they could often hold jobs, maintain relationships, and function in society, at least on the surface. The paranoia was the star of the show, with delusions often centering around themes of persecution ("The FBI is monitoring my every move"), conspiracy ("My coworkers are poisoning my coffee"), or grandiosity ("I'm actually a secret royal heir"). But here's the kicker—while the paranoia was intense, other symptoms like disorganized speech or catatonic behavior were minimal or absent.
Why the DSM-5 Eliminated Paranoid Schizophrenia as a Separate Diagnosis
So why did the powers that be decide to axe paranoid schizophrenia as a standalone diagnosis in the paranoid schizophrenia dsm 5 framework? Well, it wasn't just to make things more confusing (though we'll admit it kinda did). The research showed that these subtypes weren't stable over time—patients would often shift from one subtype to another, making the categories more like revolving doors than useful diagnostic tools. Plus, treatment approaches didn't really differ based on subtype; whether you had paranoid, disorganized, or catatonic features, the core treatment remained antipsychotic medication and psychosocial support. The DSM-5 committee figured that instead of pigeonholing people into subtypes that didn't hold up, it made more sense to diagnose schizophrenia broadly and then specify the current symptom profile. This approach allows for more flexibility in capturing how symptoms change over time, which is especially important given that paranoid schizophrenia dsm 5 presentations can evolve significantly throughout a person's illness course.
Current DSM-5 Criteria for Schizophrenia Diagnosis
Alright, let's get down to brass tacks—what does it actually take to get a schizophrenia diagnosis under the current paranoid schizophrenia dsm 5 guidelines? The DSM-5 requires two or more of the following symptoms to be present for a significant portion of time during a one-month period (with some signs of disturbance persisting for at least six months): delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior, and negative symptoms (like diminished emotional expression or avolition). At least one of those symptoms must be delusions, hallucinations, or disorganized speech. The symptoms must cause significant impairment in social, occupational, or other important areas of functioning, and they can't be better explained by another mental disorder or substance use. Oh, and here's the important part—schizoaffective disorder and depressive or bipolar disorder with psychotic features must be ruled out. The diagnosis also includes specifiers for current severity and course, which is where those paranoid features would be noted in the paranoid schizophrenia dsm 5 context.
Recognizing Paranoid Features in Current Schizophrenia Diagnoses
Even though paranoid schizophrenia isn't a separate diagnosis anymore in the paranoid schizophrenia dsm 5 framework, paranoid features are still very much a thing—and they're often the most prominent and distressing symptoms for many people with schizophrenia. These paranoid features typically manifest as persecutory delusions (believing you're being targeted, harassed, or conspired against), referential delusions (thinking random events or objects have personal significance), or paranoid hallucinations (hearing voices that are threatening or critical). The key difference now is that instead of saying "you have paranoid schizophrenia," clinicians would diagnose "schizophrenia with prominent paranoid features" or specify the current symptom profile. This approach acknowledges that paranoia might be the dominant theme right now, but it could shift over time—which is actually pretty common in the paranoid schizophrenia dsm 5 experience. Symptoms can wax and wane, and what starts as primarily paranoid might later include more disorganized or negative symptoms.

Common Signs and Symptoms of Paranoid Schizophrenia Presentation
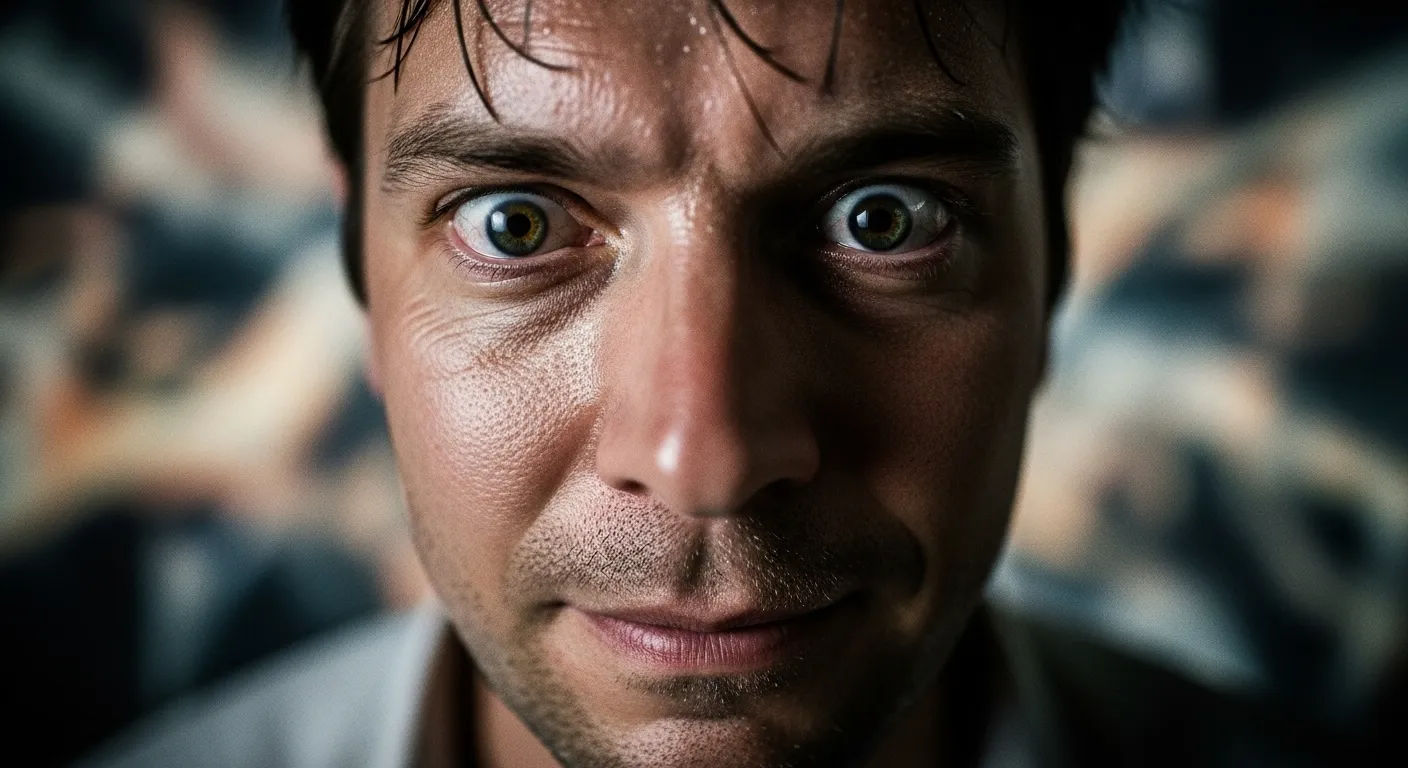
Let's talk about what paranoid schizophrenia actually looks like in real life, because Hollywood has done a real number on this one. When we're dealin' with paranoid schizophrenia dsm 5 presentations, the most obvious signs are usually the delusions and hallucinations. Persecutory delusions might have someone convinced they're being followed, spied on, or poisoned. Referential delusions could make them think the TV news anchor is sending them secret messages or that license plates contain coded warnings. Auditory hallucinations often involve voices that are critical, threatening, or commanding—sometimes telling the person to do harmful things. But here's what people often miss: the paranoia isn't just about external threats. It can also manifest as intense suspicion of loved ones, refusal to eat food prepared by others (fear of poisoning), or extreme social isolation. And while cognitive functioning might be relatively preserved compared to other schizophrenia presentations, the constant state of hypervigilance and fear takes a serious toll on daily functioning. The paranoid schizophrenia dsm 5 experience is exhausting—imagine living in a world where you can't trust anyone, where every glance feels like a threat, and where your own mind is constantly feeding you terrifying scenarios.
The Diagnostic Process: How Clinicians Assess Schizophrenia
Diagnosin' schizophrenia—whether it presents with paranoid features or not—isn't like takin' a blood test or gettin' an X-ray. There's no single lab test or scan that can definitively say "yep, this is schizophrenia." Instead, the diagnostic process for paranoid schizophrenia dsm 5 presentations involves a comprehensive clinical assessment that can take several sessions. First, there's usually a thorough psychiatric evaluation where the clinician asks about symptoms, their duration, and their impact on daily life. They'll also want to know about family history, substance use, and any previous mental health treatment. Medical tests might be ordered to rule out physical conditions that could mimic schizophrenia symptoms (like thyroid disorders or brain tumors). Sometimes neuropsychological testing is used to assess cognitive functioning. The clinician will also observe the person's behavior, speech patterns, and emotional responses during the evaluation. Family members or close friends might be interviewed (with permission) to get a more complete picture, since people with paranoid features might not always recognize or report their symptoms accurately. The whole process is designed to be thorough but also compassionate—after all, we're talkin' about someone's lived experience, not just checkin' boxes on a paranoid schizophrenia dsm 5 criteria list.
Differential Diagnosis: Conditions That Mimic Paranoid Schizophrenia
Here's where things get tricky—lots of conditions can look like paranoid schizophrenia at first glance, which is why differential diagnosis is so crucial in the paranoid schizophrenia dsm 5 assessment process. Delusional disorder might present with similar paranoid beliefs, but without the other schizophrenia symptoms like hallucinations or disorganized thinking. Schizoaffective disorder includes both psychotic and mood symptoms, so if someone has prominent depression or mania alongside their paranoia, that might be the better diagnosis. Substance-induced psychotic disorder can mimic schizophrenia symptoms, especially with stimulants like methamphetamine or hallucinogens. Medical conditions like brain tumors, epilepsy, or autoimmune disorders can also cause psychotic symptoms. Even severe anxiety disorders or PTSD can sometimes present with paranoid thinking. The key is that schizophrenia diagnosis requires ruling out these other possibilities—and that's not always easy, especially when someone is in the midst of an acute psychotic episode. That's why longitudinal assessment (following someone over time) is so important in the paranoid schizophrenia dsm 5 diagnostic process; it helps clinicians see the full picture rather than just a snapshot.
Treatment Approaches for Schizophrenia with Paranoid Features
Treatment for schizophrenia with paranoid features ain't one-size-fits-all—it's more like a custom-tailored suit that needs constant adjustments. The cornerstone of treatment is usually antipsychotic medication, which can help reduce the intensity and frequency of delusions and hallucinations. Second-generation (atypical) antipsychotics like risperidone, olanzapine, or quetiapine are often first-line treatments, though finding the right medication and dose can take some trial and error. For the paranoid schizophrenia dsm 5 presentation specifically, medications that target positive symptoms (delusions, hallucinations) are particularly important. But medication alone isn't enough—psychosocial interventions are crucial too. Cognitive behavioral therapy for psychosis (CBTp) can help people challenge and reframe their paranoid thoughts. Family therapy can educate loved ones about the illness and improve communication. Social skills training, vocational rehabilitation, and supported employment programs can help with the practical challenges of daily living. And for those with severe symptoms or safety concerns, coordinated specialty care programs provide intensive, team-based treatment. The goal isn't necessarily to eliminate all symptoms (though that would be nice), but to help people manage their illness and live meaningful lives despite the paranoid schizophrenia dsm 5 challenges they face.
| Treatment Component | Typical Cost Range (USD) | Effectiveness for Paranoid Features |
|---|---|---|
| Antipsychotic Medication (Monthly) | $50-400 | High (60-70% symptom reduction) |
| Individual Therapy (Per Session) | $100-200 | Moderate to High |
| Family Therapy (Per Session) | $150-250 | Moderate |
| Case Management (Monthly) | $200-500 | Moderate |
Living with Schizophrenia: Support Systems and Recovery
Recovery from schizophrenia—whether it presents with paranoid features or not—isn't about "getting cured" and goin' back to who you were before. It's about learnin' to live well with the illness, findin' meaning and purpose despite the challenges, and buildin' a life that feels worthwhile. For those dealin' with paranoid schizophrenia dsm 5 presentations, this often means developin' strategies to manage paranoid thoughts when they arise, learnin' to distinguish between real threats and illness-driven fears, and buildin' a support system that understands the unique challenges of living with paranoia. Peer support groups can be invaluable—there's something powerful about connectin' with others who truly get what you're goin' through. Family education and support are crucial too; when loved ones understand the illness, they can provide better support without accidentally feedin' into paranoid beliefs. Community resources like clubhouses, supported housing, and vocational programs can provide structure and purpose. And let's not forget self-care—things like regular sleep, healthy eating, exercise, and stress management can all help stabilize symptoms. The journey isn't easy, but with the right support and treatment, many people with schizophrenia—including those with prominent paranoid features—can lead fulfilling, meaningful lives. For more insights into mental health topics, visit Twitch Documentary, explore our Mental category for comprehensive resources, or read our personal account in Living With A Paranoid Schizophrenic Tips.
Frequently Asked Questions
What is paranoid schizophrenia in DSM-5?
In DSM-5, paranoid schizophrenia is no longer a separate diagnosis. Instead, the DSM-5 consolidated all schizophrenia subtypes (including paranoid, disorganized, catatonic, residual, and undifferentiated) into a single diagnosis of schizophrenia. When someone presents with prominent paranoid features—such as persecutory delusions, referential delusions, or paranoid hallucinations—the diagnosis would be schizophrenia with specification of current symptom profile. The paranoid schizophrenia dsm 5 framework now focuses on the overall schizophrenia diagnosis while noting which symptoms are most prominent at any given time, allowing for more flexibility as symptoms may change throughout the illness course.
How do they diagnose paranoid schizophrenia?
Since paranoid schizophrenia is no longer a separate diagnosis in DSM-5, clinicians diagnose schizophrenia based on specific criteria: two or more symptoms (delusions, hallucinations, disorganized speech, grossly disorganized behavior, or negative symptoms) present for a significant portion of one month, with at least one being delusions, hallucinations, or disorganized speech. The symptoms must cause significant functional impairment and persist for at least six months. The diagnostic process for paranoid schizophrenia dsm 5 presentations involves comprehensive psychiatric evaluation, medical testing to rule out other conditions, observation of behavior and speech patterns, and often interviews with family members. Clinicians also assess for paranoid features specifically, noting persecutory or referential delusions and paranoid hallucinations as part of the overall symptom profile.
What are the signs of paranoid schizophrenia?
The primary signs of paranoid schizophrenia presentations include persecutory delusions (believing one is being targeted, harassed, or conspired against), referential delusions (thinking random events have personal significance), and paranoid auditory hallucinations (hearing threatening or critical voices). Other common signs include intense suspicion of others, refusal to eat food prepared by others due to fear of poisoning, extreme social isolation, hypervigilance, and difficulty trusting even close family members. While cognitive functioning may be relatively preserved compared to other schizophrenia presentations, the constant state of paranoia significantly impacts daily functioning. In the current paranoid schizophrenia dsm 5 framework, these symptoms would be noted as prominent features within the broader schizophrenia diagnosis rather than defining a separate subtype.
Why is paranoid schizophrenia no longer a diagnosis?
Paranoid schizophrenia is no longer a separate diagnosis in DSM-5 because research showed that the schizophrenia subtypes weren't stable or clinically useful. Patients often shifted between subtypes over time, making the categories unreliable for diagnosis or treatment planning. Additionally, treatment approaches didn't differ significantly based on subtype—all forms of schizophrenia generally required antipsychotic medication and psychosocial support. The DSM-5 committee determined that a single schizophrenia diagnosis with specifiers for current symptom profile would be more flexible and accurate. This change in the paranoid schizophrenia dsm 5 framework allows clinicians to capture how symptoms evolve over time rather than locking patients into rigid categories that didn't reflect the reality of their illness experience.
References
- https://www.psychiatry.org/psychiatrists/practice/dsm
- https://www.nimh.nih.gov/health/statistics/schizophrenia
- https://www.mayoclinic.org/diseases-conditions/schizophrenia/symptoms-causes/syc-20354443
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5579659/